Diabetes is a chronic health condition that affects how the body processes blood sugar (glucose), which is the primary source of energy for cells. When unmanaged, it can lead to serious complications such as heart disease, kidney damage, nerve issues, and vision problems. According to global health data, over 500 million adults live with diabetes worldwide, with numbers projected to rise significantly by 2045. The condition arises when the pancreas doesn't produce enough insulin (a hormone that regulates blood sugar) or when the body can't effectively use the insulin it produces.
Diabetes is a chronic health condition that affects how the body processes blood sugar (glucose), which is the primary source of energy for cells. When unmanaged, it can lead to serious complications such as heart disease, kidney damage, nerve issues, and vision problems. According to global health data, over 500 million adults live with diabetes worldwide, with numbers projected to rise significantly by 2045. The condition arises when the pancreas doesn't produce enough insulin (a hormone that regulates blood sugar) or when the body can't effectively use the insulin it produces.
Types of Diabetes
There are several main types of diabetes, each with distinct causes and management approaches:
- Type 1 Diabetes: This autoimmune condition typically develops in childhood or adolescence, where the immune system attacks insulin-producing cells in the pancreas. People with type 1 diabetes require lifelong insulin therapy. Nutrition plays a supportive role in maintaining stable blood sugar levels.
- Type 2 Diabetes: The most common form, accounting for about 90-95% of cases, it often develops in adulthood due to insulin resistance and is strongly linked to lifestyle factors like obesity, poor diet, and physical inactivity. Nutrition is central to prevention, management, and sometimes reversal through weight loss and dietary changes.
- Gestational Diabetes: Occurs during pregnancy and usually resolves after birth, but it increases the risk of type 2 diabetes later in life for both mother and child. Dietary control is key during pregnancy to manage blood sugar without medication when possible.
- Other Types: Includes prediabetes (elevated blood sugar not yet at diabetic levels) and rarer forms like maturity-onset diabetes of the young (MODY) or secondary diabetes from other conditions.
Early detection through screening is crucial, as many people with type 2 diabetes remain undiagnosed until complications arise.
The Role of Nutrition in Diabetes Management
Nutrition is a cornerstone of diabetes care, helping to regulate blood glucose levels, maintain a healthy weight, and reduce risks of cardiovascular disease and other complications. A well-planned diet can improve insulin sensitivity, lower A1C (a measure of average blood sugar over 2-3 months), and enhance overall quality of life. The American Diabetes Association (ADA) emphasizes that there's no one-size-fits-all "diabetes diet"; instead, focus on personalized, sustainable eating patterns that incorporate cultural preferences and lifestyle. Recent guidelines highlight the benefits of high-fiber, plant-based foods while minimizing processed items. For type 2 diabetes, lifestyle interventions including diet can prevent or delay onset in at-risk individuals.
Key Nutritional Guidelines for Diabetics
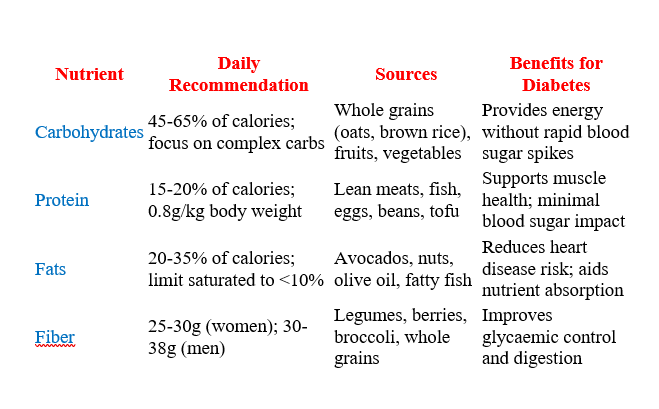
Current recommendations from leading organizations like the ADA, Mayo Clinic, and WHO stress balanced, nutrient-dense eating. Here's a breakdown:
- Calorie and Portion Control: Aim for moderate calorie intake to achieve or maintain a healthy weight. For weight loss, a deficit of 500-750 calories per day is often suggested, leading to 1-2 pounds lost weekly.
- Carbohydrate Management: Carbs have the biggest impact on blood sugar, so focus on quality over quantity. Adults with diabetes should aim for at least 14g of fiber per 1,000 calories consumed. Consistent carb intake at meals (e.g., 45-60g per meal) helps stabilize levels.
- Protein and Fats: Choose lean proteins and healthy fats. Protein should comprise 15-20% of calories, fats 20-35%, with an emphasis on unsaturated sources.
- Fiber Intake: High-fiber diets (25-30g daily) slow digestion and help control blood sugar. Sources include whole grains, vegetables, and legumes.
- Sodium and Cholesterol Limits: Keep sodium under 2,300mg/day (or less if hypertensive) and cholesterol under 200mg/day to protect heart health.
- Hydration and Alcohol: Drink plenty of water; limit alcohol to one drink per day for women and two for men, as it can affect blood sugar.
The 2025 ADA Standards of Care updated A1C goals for youth with type 2 diabetes to <6.5% for most, reflecting tighter control through diet and lifestyle
Recommended Foods and Diets
Prioritize whole, minimally processed foods. The ADA promotes patterns like the Mediterranean diet, which emphasizes vegetables, fruits, nuts, seeds, whole grains, and healthy fats, shown to improve blood sugar and heart health. Other effective diets include:
- Low-Carb Diets: Reducing carbs to 50-130g/day can aid weight loss and blood sugar control, but consult a professional to avoid nutrient gaps.
- Plant-Based Diets: High in fiber and antioxidants, these include vegetarian or vegan options with legumes, nuts, and veggies.
Recommended Foods:
- Non-Starchy Vegetables (e.g., spinach, broccoli, peppers): Unlimited; fill half your plate.
- Whole Fruits (e.g., berries, apples): 2-3 servings daily; better than juice.
- Whole Grains (e.g., quinoa, barley): 3-6 servings; choose low-glycemic options.
- Lean Proteins (e.g., chicken, turkey, fish like salmon): 2-3 servings.
- Healthy Fats (e.g., nuts, seeds, olive oil): In moderation.
- Low-Fat Dairy (e.g., yogurt, milk): 2-3 servings for calcium.
A sample daily pattern from the Dietary Guidelines aligns with diabetes needs: emphasize veggies, fruits, grains, dairy, proteins, and oils while limiting added sugars, saturated fats, and sodium.
Foods to Avoid or Limit
Certain foods can spike blood sugar or contribute to weight gain and heart issues:
- Sugary drinks (soda, energy drinks).
- Refined carbs (white bread, pastries).
- Fried foods and trans fats (chips, fast food).
- Processed meats (bacon, sausages).
- High-sodium items (canned soups, snacks).
- Excessive sweets and desserts.
Minimizing these aligns with WHO advice to avoid sugar and saturated fats for prevention.
Meal Planning Methods
Effective strategies include:
- Plate Method: Half non-starchy veggies, quarter protein, quarter carbs. Add a fruit or dairy side.
- Carb Counting: Track grams per meal; use apps or labels.
- Glycemic Index (GI): Choose low-GI foods (e.g., oats GI ~55) over high-GI (e.g., white rice GI ~73) for steadier blood sugar.
Sample 1,500-Calorie Menu (from Mayo Clinic):
- Breakfast: 1 slice whole-wheat toast with 2 tsp peanut butter, 1/2 banana, coffee.
- Lunch: Grilled chicken salad with mixed greens, tomatoes, 1 tbsp olive oil dressing, 1 small pear.
- Dinner: Baked salmon, 1/2 cup quinoa, steamed broccoli, unsweetened tea.
- Snacks: Handful of almonds; low-fat yogurt.
Eat at regular times to match medication and activity.
Additional Tips and Considerations
- Monitoring: Check blood sugar regularly and adjust diet based on readings. Work with a registered dietitian for personalization.
- Physical Activity: Combine with 150 minutes of moderate exercise weekly for better outcomes.
- Cultural Adaptations: Incorporate traditional foods healthily, like using spices instead of salt.
- Challenges: Address food insecurity through resources like community programs.
- Updates: Guidelines evolve; for 2025, focus on fiber-rich, minimally processed foods.
Conclusion
Managing diabetes through nutrition empowers individuals to lead healthier lives, preventing complications and improving well-being. By adopting balanced eating patterns, monitoring intake, and staying active, many can achieve better control. Always consult healthcare providers for tailored advice, as individual needs vary. Resources from the ADA, Mayo Clinic, and WHO provide ongoing support for sustainable changes.